Cervical
Insufficiency
-
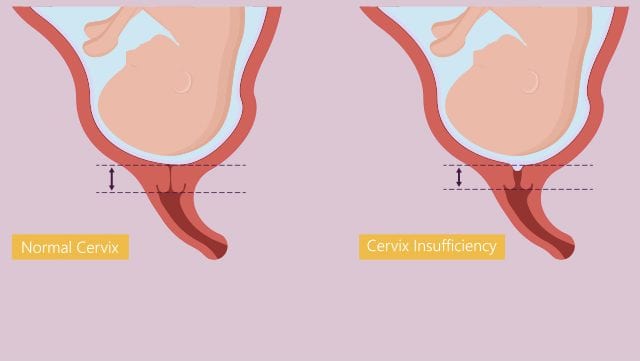
Recurrent painless cervical dilatation leading
to second trimester loses
-
“The inability of the uterine cervix to
retain a pregnancy in the 2nd trimester in the absence of clinical contractions,
labor or both”
Pathogenesis
-
Structural cervical weakness ( Leading to
recurrent 2nd trimester losses )
§
Acquired - may be secondary to cervical surgery
or uterine surgery
o
(Dilatation , curettage , hysteroscopy )
§
Congenital
o
Nonrecurrent 2nd trimester looses
§
Decidual infection /inflammation
§
Bleeding at the surface between decidua and
placenta
§
Uterine over distension
Clinical findings
-
History of Recurrent 2nd Trimester pregnancy
losses or live births (often before 24 weeks )
-
No / minimal mid symptoms
-
Cervical dilation or effacement on physical
examination
RISK FACTORS
-
Cervical trauma (most common) = during labor (spontaneous
or iatrogenic), mechanical dilation during gynecologic procedure, tumor treatment
-
Congenital cervical anomalies(rare) genetic
disorder affecting collagen synthesis (Ehlers Danlos Syndrome), uterine anomalies,
in vitro Diethylstilbesterol
-
Short cervical length –detected on transvaginal
USG
SYMPTOMS
Begins at 14 to 20 weeks of Gestations
-
Braxton Hicks Contractions
-
Pelvic pressure
-
Premenstrual like cramping / backache
-
Change in vaginal discharge (Volume increase,
thickness decrease, color change from normal (white, light yellow) to pink, tan,
red spotting)
EXAMINATIONS
-
Cervix = soft, closed with minimal effacement
-
Tocodynamometry = no infrequent contractions
-
Provocative maneuvers (Supra pubic pressure , fundal
pressure or Valsalva maneuver ) reveals
fetal membrane in the canal( membrane may prolapse )
Imaging
-
Transvaginal USG (TVU)
(CL <= 25mm)
-
Debris (sludge or biofilm), SLUDGE = fetal squames,
vernix, leukocytes, bacteria
-
On Serial USG, CL may decrease
Diagnosis
Past History
§
Past history of >2 consecutive second trimester
losses or extremely low term (mostly loss before 24 weeks)
Ultrasound Based diagnosis
§
Obstetrics history of second trimester loss or
premature delivery (<28 weeks) and short CL in TVU
§
Serial USG shows CL <= 25 mm in 24 weeks
§ Infections,
labor, bleeding excluded
Physical Examination
-
Usually in patients in between 14 to 27 weeks of
Gestation
-
Physical examinations= effacement in absence of labor,
advanced cervical dilation
-
Membrane may be prolapsed or rupture
-
Labor, infection, and bleeding related to
placental abruption or placenta previa should be excluded
-
Exclusion of other differential diagnosis
Diagnosis Exclusion Technique
-
Labor – Tocodynamometry
-
Infection – Urine culture /Urinalysis Culture
and amniocentesis (when uterine dilation or membrane effacement confirmed on examination)
-
Bleeding – history, physical and
ultrasound examinations
When to perform Amniocentesis?
-
When cervix dilated >=2cm or manual or
speculum examination (incidence of intraamniotic infection = 20 to 50 %)
-
USG= inflammation finding (debris /sludge /biofilm)
-
Membrane visible or exposed at external Os